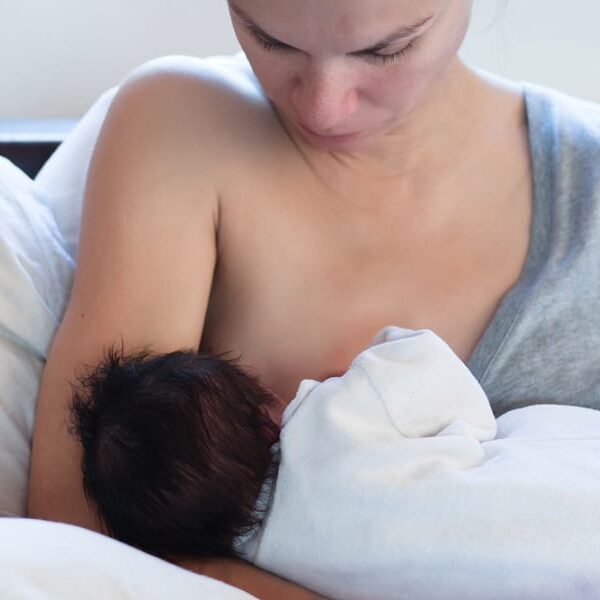
Breastfeeding
I Hate Breastfeeding! And Other Confessions from Nursing Moms
Updated 11/17/20
Be honest. Sometimes we just don’t love the things we think we will love about being a mom-at least not all the time.
In my work supporting women through the childbearing year, I believe that much of what we struggle with comes down to our expectations. A long labor feels difficult because we expected it should be shorter, or a short labor feels difficult because we expected it to be longer. We expect to feel contractions in our bellies instead of our backs. We often feel as if we ‘should’ feel a certain way about everything from discovering the 2nd line on the stick to what it’s like to have that pregnancy bump, to how we should feel when we meet our babies for the first time.
Those ‘shoulds’ deny us the opportunity to be truly present for our own authentic experience while we forever chase the something that we think other mothers must be feeling.
These are some of the breastfeeding issues I’ve heard about from nursing moms, or experienced myself.
Ambivalence about Breastfeeding
Breastfeeding may or may not feel like the sweet or fabulous thing you expected it to be. I find that most mothers experience some ambivalent feelings about breastfeeding during the first days and weeks, even in the absence of complications.
Your hormones and hormone receptors are starting to establish strong little paths of connection that bring together the sensory experiences of seeing your baby, having skin to skin contact, rooting and latching sensations, and the letdown trigger that ejects milk from where it has been stored in the glandular tissue of the breast. This cascade of events culminates in that mother-love glow we get from oxytocin. Until this path is established, however, you may not think this is the coolest thing you’ve ever done. It’s a little like expecting a great runner’s high after the first time you put on running shoes and complete the first few blocks of an uncomfortable jog. Give yourself some time and be patient with yourself when you are feeling ambivalent or discouraged about nursing. It passes! If you are not feeling confident that your baby is getting what he/she needs, if you’re experiencing any pain or discomfort, or feel that the ambivalence isn’t resolving, call a lactation consultant. Learn when and why you should reach out for help. As breastfeeding experts, we can also help you resolve the challenges that are getting in the way and can help you make so many aspects of this more manageable.
Nursing makes me feel anxious or sad: Breastfeeding dysphoria
A small percentage of women respond to breastfeeding hormones with a sudden onset of feeling sad, angry, homesick, or anxious. Often identified at D-MER (Dysphoric Milk Ejection Reflex), this condition is thought to be caused by the rise in prolactin levels, which briefly competes with and reduces dopamine levels. Brought on by suckling and/or letdown, the reflexive sensation is brief and usually lasts from 30 seconds to no more than a few minutes. The sensation can be mild, moderate or severe. Because this is often not expected it can be difficult to take in. One minute you’re having a sweet moment of cuddling your baby and readying to latch and the next you’re feeling waves of emotional distress that seem to have no identifiable cause. Women can also experience dysphoria during other hormonal events, such as orgasm. I recommend reaching out to learn more to better understand these phenomena and to find ways to get some relief. There are treatment options.
Breastfeeding turns me on. Arousal and breast stimulation
The nipple and areola are highly enervated and are designed to trigger a cascade of hormonal events. The felt sensation of nipple stimulation outside of sexual activity is new for many first time moms. In the early days the nipple is extremely sensitive, ensuring that the body does what it needs to in response to nursing. Over time, most women notice a significant reduction in the intensity of the sensation.
The stimulation of suckling is designed to release oxytocin. Oxytocin does all kinds of cool things: ejects milk, causes uterine contractions that encourage fertilization on the front end and gets babies out in labor at the end of pregnancy. Oxytocin aids in digestion and healing, increases blood flow, makes our pupils dilate, leads us to trust, and causes orgasm. Now more than ever before, we have a better understanding about arousal and orgasm itself, which has led to more honest dialogue about this felt experience. Orgasmic birth and orgasmic breastfeeding are not at all uncommon.
Having these uterine contractions and increased blood flow actually happens in all women to some degree. It’s lifesaving. It’s a key factor in helping prevent excessive bleeding in the uterus and it helps tender tissues to mend.
I hope that reframing these sensations with some of the broader views mentioned here reassures and supports you.
There is absolutely nothing wrong with you. Using mindfulness practices can help you notice the physiological sensations while loosening the thought train of associations that make you feel uncomfortable. It is what it is. And it’s good for you!
I want to stop breastfeeding. And then I don’t. Conversations about Weaning
Another area where our ideas about nursing can collide with our felt experience occurs around weaning. Maybe you were sure that you would not be nursing your baby past their first (or second, or third) birthday, or maybe you expected to nurse longer but your growing little one is too busy to give you the time of day. Maybe you feel completely ready to quit after a rough week after you’ve gone back to work and the weekend comes and you find yourself heartbroken when you think your baby just refused the breast.
Here is my best advice about this whole topic: sometimes it’s baby led, sometimes mother led, and more often than not it’s something you have to feel out and just trust the both of you. Give yourself time to explore what is authentic when you factor in all the preconceptions you have, the opinions of others, all the moods (your own and your baby’s!), and the developmental changes your little one is experiencing. Recognize that it’s not an all or nothing proposition; even relactation is available to you if you feel that the timing just wasn’t right for you and your baby when you made the choice to wean. For your breast health and for your baby’s health, talk to a lactation consultant. She can help you manage your breast health and your baby’s needs throughout the whole process.
Contact us for a guilt-free exploration of what support services might be most impactful for you right now.